Good bacteria for bad wounds
Millimeter by millimeter, new tissue makes its way through a wound until it has closed a skin lesion. Soon, in the best case, there is nothing left to see of a knee scrape, a finger cut or a burn blister. Not so with chronic wounds, though: If the injury has not healed after four weeks, there is a wound healing disorder. Sometimes, seemingly harmless tissue damage can develop into a permanent health problem or even blood poisoning.
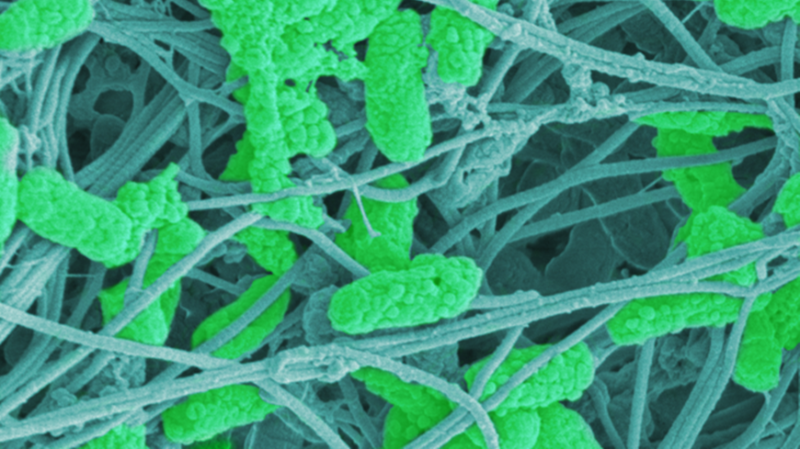
Treatment is particularly difficult because germs that know how to protect themselves perfectly settle here. These bacteria form a biofilm, a stubborn compound of various pus pathogens. For their own protection, they produce a layer of mucus with which they attach themselves to surfaces. Antibiotics or disinfectants reach their limits because they cannot get to the dangerous germs. A team from Empa and the Massachusetts Institute of Technology (MIT) in Boston is currently developing a wound dressing that uses "good" probiotic bacteria to combat biofilms. The researchers recently published a proof of concept in the journal Microbes and Infection.
Tenacious biofilm
The team led by Empa researchers Qun Ren from the Biointerfaces laboratory in St. Gallen used living probiotic bacteria for the new dressing. They are found in healthy intestinal flora and play a major role in the production of foods such as yogurt and cheese. "The used probiotic lactobacilli are biocompatible and create an acidic environment by producing lactic acid," says medical doctor Zhihao Li, who contributed clinical expertise to the project as a visiting scientist at Empa. This, he says, is intended to push the unfavorable, alkaline pH in chronic wounds in the right, i.e. acidic, direction. "In our laboratory experiments, the bactria were able to induce a strongly acidic pH of 4 in the culture medium," Qun Ren said. At the same time, the probiotics promoted the migration of human fibroblasts under the investigated conditions.
Beneficial bacteria
Finally, the beneficial bacteria were integrated into a dressing that protects chronic wounds from further infection. This also allowed the living lactobacilli to produce lactic acid in a protected environment. As desired, the dressing released the acidic product into the environment in a controlled and steady manner. In laboratory tests, the dressing material with integrated probiotics was able to completely remove a typical biofilm of skin pathogens in a culture dish. The question now was: Do the dressing containing beneficial bacteria also pass the test with human skin?
The living bandage
The researchers created artificial wounds with a diameter of two millimeters on small tissue samples and allowed a biofilm of wound pathogen Pseudomonas aeruginosa to grow. In this three-dimensional model of a human skin infection, the probiotics-containing dressing reduced the number of pathogens by 99.999 %. In addition, the researchers were able to prove that the probiotics do not harm human skin cells and triggers the production of inflammatory response of the cells. After this proof of concept, says Qun Ren, further analyses of the mechanism of action will help to exploit the potential of the beneficial bacteria for a "living" dressing.